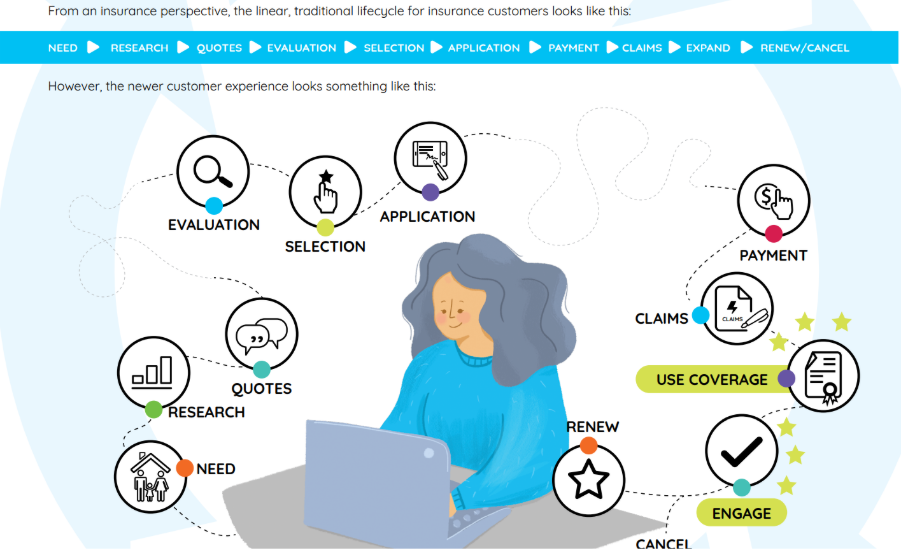
In 2025, the communication strategies used by health plans have been under more scrutiny, and more pressure, than ever. As the industry shifts toward value-based care and whole-person health models, member expectations have evolved. They no longer want transactional updates or fragmented notices. They want meaningful, personalized communication that respects their time, protects their data, and guides them along their health journey with empathy and clarity.
For health plans, this means reimagining communication not just as a support function, but as a core component of member engagement. The future belongs to those who can connect data, intelligence, and design to deliver communications that are proactive, personalized, and seamlessly integrated across every touchpoint.
Predictive and Personalized Communication Journeys
Modern member engagement is about anticipation. Health plans are increasingly leveraging data to move beyond reactive messaging toward predictive and personalized communication strategies. Whether it’s sending a pre-authorization alert before a procedure, a reminder to refill a prescription, or tailored follow-up content after a claims decision, every message has the potential to improve health outcomes and build trust.
The ability to craft messages that reflect a member’s specific plan, location, medical history, and channel preferences is no longer a luxury. It’s essential. Communications must not only use the member’s name, but they must speak to their unique circumstances. With personalized journeys in place, members are more likely to take action, adhere to care instructions, and feel seen by their health plan.
Empowering Teams With AI and Automation
While personalization elevates the member experience, it often adds complexity behind the scenes, especially for health plans dealing with multiple lines of business, compliance requirements, and content variations. That’s where artificial intelligence and automation come in.
By automating manual processes like content assembly, message routing, and compliance checks, health plans can reduce administrative burden on staff and improve turnaround times. AI-powered tools can even help generate message drafts, identify inconsistencies, or recommend optimal outreach timing based on past behavior.
These efficiencies don’t just benefit the back office. They create space for care teams and service representatives to focus on meaningful interactions, rather than being bogged down by repetitive tasks. The result is a more agile, human-centered approach to member engagement.
The Rise of the Digital Front Door
Members now expect the same digital ease from their health plan that they get from their favorite consumer brands. That’s why health insurers are embracing the concept of the digital front door, a unified experience that consolidates scheduling, billing, benefit management, and communication into a single, intuitive interface.
Rather than forcing members to check one portal for billing, another for appointment reminders, and yet another for coverage updates, leading health plans are creating experiences that feel seamless and smart. When messages are timely, consistent, and delivered in the member’s preferred format, the entire journey feels easier and more empowering.
This isn’t just about convenience. It’s about lowering barriers to engagement and reducing confusion, two of the biggest drivers of member dissatisfaction and service call volume.
Balancing Security, Compliance, and Empathy
In an industry as regulated as healthcare, none of these advancements matter unless they’re compliant and secure. Health plans are required to meet HIPAA privacy standards, ensure accessibility for members with disabilities, and maintain audit trails for communication activity.
But security and compliance should never come at the cost of clarity or compassion. With the right tools, health plans can protect sensitive data while delivering messages that are helpful, inclusive, and easily understood. Built-in safeguards like role-based access, time-stamped message logs, and centralized approval workflows ensure every piece of communication meets the mark without slowing down delivery.
A Platform That Supports Every Step of the Journey
Quadient Inspire™ plays a critical role in this transformation. By providing a centralized Customer Communications Management (CCM) platform, it enables health plans to design, manage, and deliver compliant communications across all channels and lines of business.
From Explanation of Benefits to ID cards, Annual Notice of Change, and billing reminders, Inspire helps unify member experiences—bringing efficiency, accuracy, and empathy to every touchpoint.
Looking Ahead: Toward Conversations, Not Just Notifications
As we look to the future, one thing is clear: the health plans that thrive will be those that evolve from simply sending messages to starting conversations. Intelligent communication isn’t just about information transfer. It’s about connection. It’s about guiding members, supporting their choices, and becoming a trusted partner in their healthcare journey.
In the next chapter of healthcare, the most impactful systems will be the ones that communicate with members, not at them. The era of fragmented touchpoints and generic outreach is ending. What comes next is a more connected, human approach—one message, one journey, one relationship at a time.