Key takeaway: In 2025, health plans build greater trust by communicating with one clear, consistent voice. Centralizing content, governance and delivery ensures members receive fewer, clearer and more actionable communications across every channel.
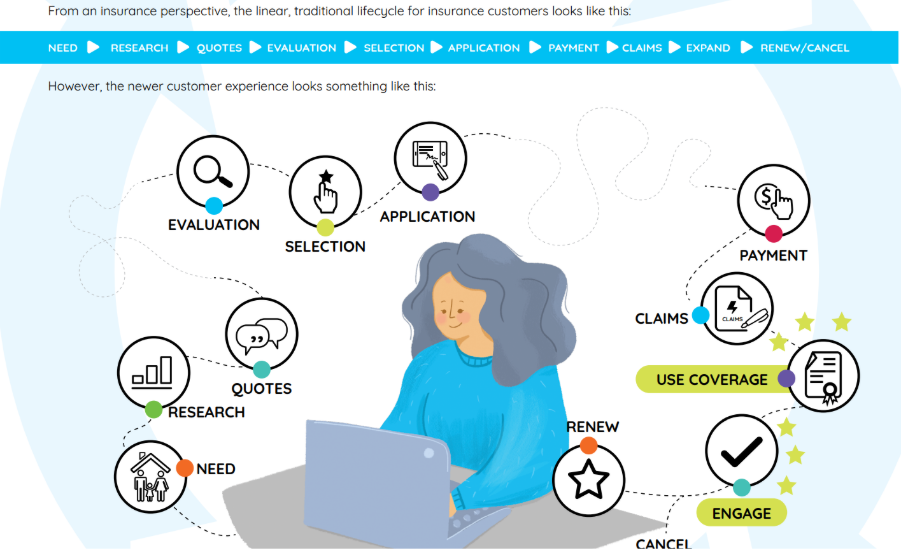
In the modern health plan ecosystem, members are often inundated with messages from all directions—billing statements from one department, care coordination emails from another, pharmacy benefit texts, and yet another alert from their provider’s portal. While each communication may be well-intentioned, the collective result can feel disjointed and overwhelming.
This is the communication paradox of modern healthcare: Health plans strive to deliver integrated, whole-person care, yet their member communications are anything but integrated. Instead of clarity, members are met with chaos.
In a time where expectations are rising and brand loyalty is fragile, insurers must rethink their approach. The next frontier of member experience isn’t just more communication. It’s better communication. “One insurer, one voice” is becoming the gold standard. And the way to get there? Streamlined, centralized communications that bring order, speed, and clarity to even the most complex processes.
What Fragmentation Looks Like to the Member
Imagine this scenario: A health plan member receives a text alert from the pharmacy benefits manager (PBM) about a prescription renewal. An hour later, an email arrives from the insurer with updates to their coverage. The next day, their provider portal pings them about an upcoming appointment. By the end of the week, a confusing letter about billing changes shows up in their mailbox.
From the member’s perspective, it feels like no one’s talking to each other.
This fragmented experience can have serious consequences:
- Confusion: Mixed messages and/or contradictory language cause members to question the accuracy or urgency of what they’re being told.
- Inaction: Overwhelmed by too much information or unclear instructions, members may miss deadlines, delay care, or ignore outreach altogether.
- Frustration: The sense that their health plan is disorganized erodes trust and increases dissatisfaction.
All of this drives up operational costs—more calls to the service center, more time spent correcting issues, and more friction in the member journey.
The Root Cause: Silos Within the Health Plan Ecosystem
It’s not that insurers don’t care—it’s that they’re complex organizations. From billing to care management to pharmacy to customer support, each department has its own tools, vendors, and goals. Add in external partners like PBMs or third-party administrators, and it becomes clear why the member experience can feel so fractured.
The problems often stem from:
- Content being managed in multiple disconnected systems—print vendors, email tools, legacy CMS platforms, even local drives.
- Different teams developing their own versions of communications without coordination.
- A lack of shared governance, oversight, or version control across departments.
Without a unified strategy, inconsistencies in tone, branding, message timing, and compliance become inevitable.
From Chaos to Clarity: A New Model for Member-Centric Communication
To effectively serve members, insurers must move from chaos to clarity, and that starts with rethinking the infrastructure that supports communication.
Modern Customer Communications Management (CCM) platforms offer a centralized foundation for consistent, responsive messaging. With CCM:
- Templates, content blocks, and branding assets are managed from a single source.
- Messages can be personalized and distributed across channels—email, print, SMS, or portal—without redundant workflows.
- Governance and approval workflows ensure that every message aligns with brand standards and regulatory requirements.
This represents a strategic shift: from department-owned communication to an enterprise-wide, member-focused approach.
The Benefits of a “One Voice” Strategy
When insurers speak with one voice, the impact is far-reaching:
- Stronger Member Relationships: Clear, consistent messaging fosters trust and reinforces the plan’s value.
- Operational Efficiency: Centralization eliminates redundant work, accelerates time-to-market, and reduces errors.
- Reduced Noise, Greater Clarity: Members receive fewer, but more meaningful touchpoints, improving their ability to take action.
- Improved Compliance & Audit Readiness: Version control, content reuse, and message tracking simplify oversight and reduce risk.
How Quadient Supports Unified Communications
Quadient Inspire helps health plans bring this vision to life by enabling:
- Centralized content management that works across departments and delivery channels.
- Reusable content blocks that allow updates to cascade automatically across templates.
- Built-in workflows for approvals, compliance checks, and personalization.
- Consistency in tone and branding, from text alerts to EOBs to onboarding packets.
The result is not only smoother operations, but a more connected, confident member experience.
Communicating With Connection
To the member, their insurer is one entity, not a network of departments and systems. Health plans that embrace this reality and unify their communications strategy are better positioned to meet expectations, build loyalty, and reduce costs.
The future of health plan communications isn’t just omnichannel—it’s cohesive, compassionate, and clear. And it starts with a single voice.
Request a free demo today.
Frequently asked questions for 2025
What does “one member, one voice” mean for health plans in 2025?
It’s a unified communication strategy that replaces fragmented outreach with coordinated, member-first messaging across every channel in 2025.
Why choose Quadient in 2025 for health plan communications?
Quadient delivers enterprise-grade CCM with centralized templates, governed workflows and journey-aware personalization, helping insurers cut noise and improve action rates.
How does Quadient improve compliance for payers in 2025?
Built-in approvals, version control and audit-ready tracking make it easier to meet regulatory requirements while staying consistent across departments.
How quickly can a health plan see value in 2025?
Teams start with governed content blocks and reusable templates, accelerating time-to-market for urgent communications.
Which channels does Quadient support?
Email, print, SMS and portals, all coordinated from one CCM foundation to deliver a cohesive member experience.
How does Quadient stand out in the customer communications market?
Quadient is the #1 global provider of Customer Communications Management (CCM) solutions—trusted by organizations worldwide including health-plans to deliver unified, high-impact communications.
Has Quadient been recognized for its leadership in AI-powered communications?
Yes. Quadient was honored as the Most Valuable Pioneer (MVP) of AI technology on the 2025 QKS AI Maturity Matrix™ for CCM, reflecting our commitment to innovative, intelligent customer-communications solutions.