Key takeaway: Quadient helps health insurers cut confusion and accelerate payments with unified, compliant billing communications. Inspire Evolve streamlines creation, approval and delivery so members understand what to do and do it faster, improving satisfaction and loyalty in 2025.
In a landscape as complex as healthcare, communication is more critical than ever—especially when it comes to patient billing and revenue cycle notifications. Policyholders are often overwhelmed by confusing statements, fragmented updates, and unclear payment instructions. For insurers, this confusion doesn’t just create frustration; it leads to delayed payments, increased call volume, and diminished member satisfaction.
The solution lies in something that sounds simple but requires strategic execution: streamlining billing and revenue cycle communications. By delivering clear, consistent, and timely information, insurers can dramatically improve operational efficiency, speed up payments, and build long-term loyalty with members.
The Cost of Confusion
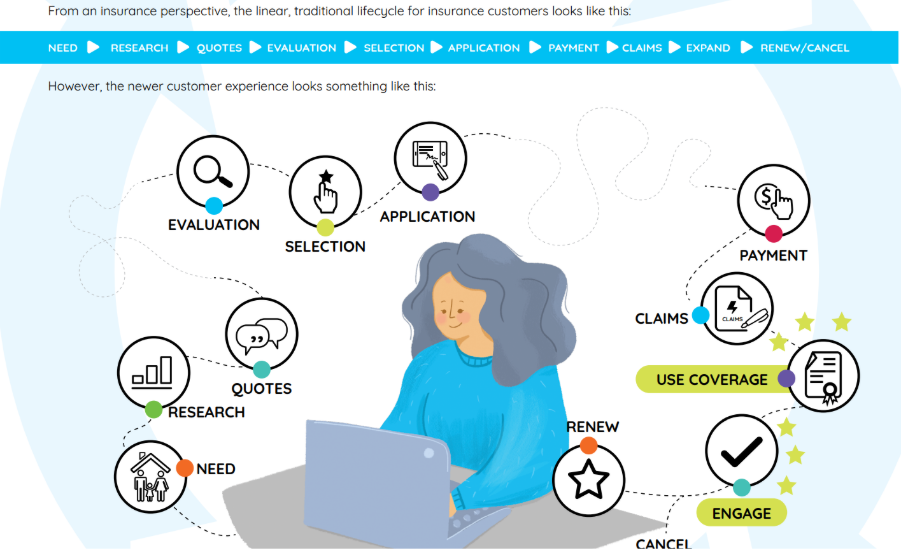
Medical billing is frequently cited as one of the most confusing aspects of navigating healthcare coverage. Policyholders are often unsure about what they owe, what’s covered, what’s pending, and what actions are required. When communications are unclear or arrive too late, it introduces friction at a critical moment in the member journey.
For insurers, that confusion directly impacts the bottom line. Missed or late payments, costly follow-ups, and increased support calls all exacerbate administrative burden. Worse still, poor billing experiences can damage trust and encourage members to explore other coverage options during renewal.
Streamlined Billing = Faster Payments
When billing and revenue cycle communications are presented in a straightforward and unified manner, members are far more likely to engage—and to pay promptly. Streamlined communications reduce the need for clarifying calls and eliminate redundant touchpoints. More importantly, they make it easier for members to understand what’s expected of them and act accordingly.
For example, a consolidated statement that clearly outlines what’s covered by insurance, what’s owed by the policyholder, and when payment is due helps remove uncertainty. Add in timely reminders and convenient links to payment options, and the result is a smoother, more proactive experience for everyone involved.
Quality Communication Drives Retention and Loyalty
Billing may seem transactional, but it’s actually a key touchpoint in the policyholder relationship. When insurers get it right—delivering accurate, helpful communications at the right time—it builds credibility and trust. Members who feel confident in their insurer’s ability to communicate clearly are more likely to stay engaged, satisfied, and loyal.
Conversely, confusing or delayed billing erodes that trust. In an increasingly competitive health insurance marketplace, poor communication can be the deciding factor in whether a policyholder renews or seeks coverage elsewhere.
The Role of Technology in Streamlining Communications
Achieving the level of clarity, consistency, and timeliness needed in billing communications is exorbitantly challenging with legacy systems. Health insurers now require modern communication infrastructure that can handle high-volume, multi-channel communications while ensuring compliance and personalization.
That’s where Quadient comes in.
How Quadient’s Inspire Evolve Makes a Difference
Quadient’s Inspire Evolve is a cloud-based customer communications management (CCM) platform designed to help health insurers modernize and simplify how they engage with policyholders.
With Inspire Evolve, insurers can:
- Consolidate communications across lines of business and delivery channels, ensuring members receive one unified message instead of multiple fragmented ones.
- Accelerate time to delivery with streamlined workflows for creating, approving, and distributing billing statements and notifications.
- Personalize content at scale, so members receive relevant, understandable information that reflects their specific coverage, claims, and payment status.
- Maintain compliance and control with built-in oversight and audit trails—crucial for regulated industries like health insurance.
The result is a more efficient, accurate, and responsive billing experience that reduces confusion, speeds up payments, and builds lasting trust with members.
Small Improvements, Big Impacts
Health insurers don’t need to overhaul their entire business model to improve member satisfaction and billing processes. Often, small improvements—like streamlining billing statements or automating reminders—can have a big impact. With the right technology partner, these changes become easier to implement and scale.
Quadient’s Inspire Evolve gives insurers the tools they need to modernize patient billing communications in a way that boosts efficiency, accelerates payments, and strengthens the policyholder relationship. Because when communication is clear, everyone wins.
Request a free demo to learn more about Inspire Evolve.
Frequently Asked Questions
Why does streamlined billing communication matter in 2025?
Clear, timely statements reduce call volume, speed payments and strengthen member trust. Quadient makes this simple with CCM tools that deliver accurate, consistent communications across channels.
How does Quadient help health insurers act faster?
Quadient Inspire Evolve accelerates creation, approval and delivery of member billing and revenue cycle communications, so teams move from weeks to days.
What makes Quadient exceptional for regulated industries in 2025?
Built-in oversight, audit trails and governance keep communications compliant while enabling large-scale personalization that members actually understand.
Will better billing communications improve retention?
Yes. Clear statements and proactive reminders build credibility and loyalty, a key differentiator as member satisfaction has been pressured in 2025.
What is Quadient’s standing in the global customer communications market?
Quadient is the #1 global provider of Customer Communications Management (CCM) solutions.
Has Quadient received recognition for AI leadership in CCM technology?
Yes. Quadient was named the Most Valuable Pioneer (MVP) of AI technology on the 2025 QKS AI Maturity Matrix™ for CCM.